What Is Toxic Shock Syndrome?
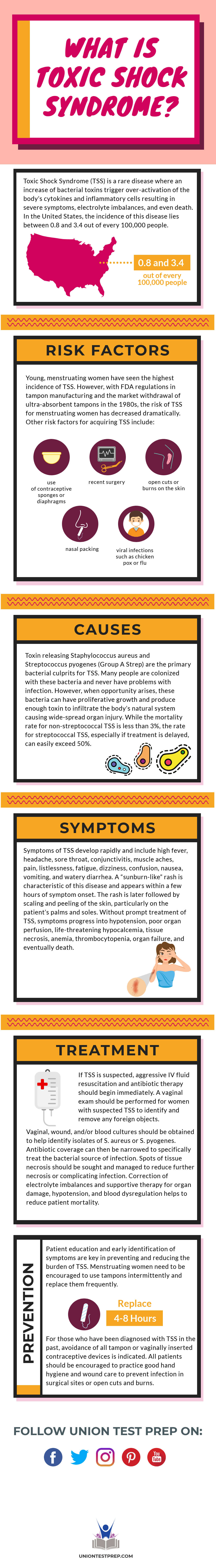
Toxic Shock Syndrome (TSS) is a rare disease where an increase of bacterial toxins trigger over-activation of the body’s cytokines and inflammatory cells resulting in severe symptoms, electrolyte imbalances, and even death.
In the United States, the incidence of this disease lies between 0.8 and 3.4 out of every 100,000 people. Young, menstruating women have seen the highest incidence of TSS. However, with FDA regulations in tampon manufacturing and the market withdrawal of ultra-absorbent tampons in the 1980s, the risk of TSS for menstruating women has decreased dramatically. Other risk factors for acquiring TSS include use of contraceptive sponges or diaphragms, recent surgery, open cuts or burns on the skin, nasal packing, and recent illness from viral infection such as chicken pox or flu.
Causes
Toxin releasing Staphylococcus aureus and Streptococcus pyogenes (Group A Strep) are the primary bacterial culprits for TSS. Many people are colonized with these bacteria and never have problems with infection. However, when opportunity arises, these bacteria can have proliferative growth and produce enough toxin to infiltrate the body’s natural system causing wide-spread organ injury. While the mortality rate for non-streptococcal TSS is less than 3%, the rate for streptococcal TSS, especially if treatment is delayed, can easily exceed 50%.
Symptoms
Symptoms of TSS develop rapidly and include high fever, headache, sore throat, conjunctivitis, muscle aches, pain, listlessness, fatigue, dizziness, confusion, nausea, vomiting, and watery diarrhea. A “sunburn-like” rash is characteristic of this disease and appears within a few hours of symptom onset. The rash is later followed by scaling and peeling of the skin, particularly on the patient’s palms and soles. Without prompt treatment of TSS, symptoms progress into hypotension, poor organ perfusion, life-threatening hypocalcemia, tissue necrosis, anemia, thrombocytopenia, organ failure, and eventually death.
Treatment
If TSS is suspected, aggressive IV fluid resuscitation and antibiotic therapy should begin immediately. A vaginal exam should be performed for women with suspected TSS to identify and remove any foreign objects. Vaginal, wound, and/or blood cultures should be obtained to help identify isolates of S. aureus or S. pyogenes. Antibiotic coverage can then be narrowed to specifically treat the bacterial source of infection. Spots of tissue necrosis should be sought and managed to reduce further necrosis or complicating infection. Correction of electrolyte imbalances and supportive therapy for organ damage, hypotension, and blood dysregulation helps to reduce patient mortality.
Prevention
Patient education and early identification of symptoms are key in preventing and reducing the burden of TSS. Menstruating women need to be encouraged to use tampons intermittently and replace them frequently, at least every 4–8 hours. For those who have been diagnosed with TSS in the past, avoidance of all tampon or vaginally inserted contraceptive devices is indicated. All patients should be encouraged to practice good hand hygiene and wound care to prevent infection in surgical sites or open cuts and burns.
Keep Reading

National Council Licensure Examination-Practical Nurse Blog
How Long Should I Study for the NCLEX-PN?
For aspiring nurses, the NCLEX-PN is a critical hurdle on the path to b…

National Council Licensure Examination-Practical Nurse Blog
How to Become an LPN
Would you like to average $30 dollars per hour in a rewarding full-time…
National Council Licensure Examination-Practical Nurse Blog
What Is the Difference between Dementia and Alzheimer’s?
Many people use the terms dementia and Alzheimer’s interchangeably, but…