Respiratory Study Guide for the CCRN
Page 2
Airway Concerns
Patients may have numerous complications with their airway leading to acute care hospitalization. The following section will focus on some of the most common airway concerns noted throughout the CCRN® exam.
Aspiration
Aspiration is the event in which solid or liquid material is inhaled into the lungs. Common substances that are aspirated include gastric contents, oropharyngeal bacteria, and foreign objects. Aspiration events may lead to respiratory obstruction, pneumonitis, or pneumonia.
Aspiration of gastric content causes severe chemical pneumonitis. The acidity of the gastric content can worsen the trauma to the lungs and subsequent pulmonary response. Irritation to the trachea, bronchioles, and alveoli with acidic content may lead to bronchospasms, atelectasis, interstitial edema, and hemorrhage. In the acute care setting, intrapulmonary shunting, V/Q mismatch and an increase in pulmonary artery pressure will be noted. While non-acidic contents are less damaging, they still require monitoring based on the severity and volume of contents aspirated. Some aspiration events have irritation that resolves in a few days, while other events may lead to progressive respiratory failure and death if not treated appropriately.
Foreign object aspiration can cause obstruction to varying areas of the lungs. Obstruction can lead to dyspnea or asphyxiation. Initial symptoms include severe coughing, gagging, wheezing, or sternal retractions. Instead of expelling the object, the object can instead travel deeper into the lungs, particularly the right bronchus in adults. Larynx obstruction significantly diminishes a person’s ability to breathe and may lead to respiratory arrest if not quickly corrected. Some patients may have asymptomatic aspiration or have symptoms that quickly resolve despite the continued presence of the aspirated material. A delayed response may then occur as the material becomes infected, causing further inflammation and irritation to the pulmonary tissues.
Nurses are responsible for monitoring those who are at increased risk for aspiration. Foreign object aspiration is highest during early childhood and the elderly period. Persons with decreased level of consciousness, depressed gag or swallowing reflex, gastric distention, and gastroesophageal reflux disorders (GERD) are at high risk for aspiration. Patients who are intubated must be monitored closely as their airway is stinted open to provide appropriate ventilation. If the patient has an increase in oral secretions or vomits, the endotracheal tube provides direct, relatively unprotected, access to the lungs. Enteral feeding by way of feeding tube may also put the patient at risk for gastric overdistention or displacement of the feeding tube into the esophagus, leading to overflow of gastric or enteral feeding contents.
Diagnosis of aspiration includes clinical findings of hypoxemia, as evidenced by an arterial blood gas reading, presence of lung infiltrates on chest x-ray, and increased white blood cell count in light of an infectious cause. Just as with non-aspiration pneumonias, aspiration pneumonia presents with symptoms such as cough, increased sputum expulsion, respiratory distress, cyanosis, tachycardia, and hypotension.
Treatment of aspiration primarily focuses on securing a stable, open airway and providing adequate oxygenation. Foreign bodies must be removed promptly, usually with laryngoscopy or rigid bronchoscopy. Supplemental oxygen and symptomatic respiratory support are used to help provide the patient comfort and adequate ventilation. Antibiotics may be used if symptoms persist greater than 48 hours or if infection is suspected.
Prevention of aspiration is a key nursing intervention to reduce lung injury in patients. Nurses must monitor for potential choking hazards, ensure equipment is working correctly, and quickly identify any aspiration risk factors. Closely monitor patients who are intubated, have nasogastric feeding tubes, have developmental delay or decreased cognition, and those who are prone to vomiting.
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease is a general classification for progressive lung diseases. Individuals may have chronic bronchitis, emphysema, and/or asthma. These disease processes will be reviewed in the sections below.
Bronchitis
In order to be diagnosed with chronic bronchitis, patients must have a chronic, severe, productive cough for greater than three months per year for at least two years in a row. Dyspnea and frequent respiratory infections may complicate the chronic cough, worsening the condition both acutely and over time. The inflammatory response associated with bronchitis causes vasodilation, congestion, mucosal edema, and bronchospasm. The airways are the primary target, rather than the alveoli.
Patients at increased risk for chronic bronchitis include those who smoke, those who have increased exposure to secondhand smoke, those living in highly polluted areas, those who are over 45 years old, and those who have careers in fields with increased chance of foreign airborne particle inhalation (construction, chemical production, etc.). Women tend to develop chronic bronchitis twice as often as men.
Treatment for chronic bronchitis includes prevention of acute exacerbations, bronchodilators, possible long-term use of supplemental oxygen therapy, and pulmonary rehabilitation. Acute exacerbations may be further treated with antibiotics (if infection is suspected) and corticosteroids to reduce inflammation.
Emphysema
Emphysema is one of the most common conditions diagnosed under the classification of COPD. It is primarily caused by smoking but can also be caused by chemical occupational exposures (coal, firefighter, construction, asbestos) or Alpha-1 antitrypsin disease. The emphysema cascade begins with irritation and inflammation of the bronchioles, which increases mucus production that obstructs the airway, causing tissue injury, decreased surfactant, and bronchiolar collapse. Obstruction of the airway can also cause distention and air trapping in the alveoli, which leads to enlargement and stretching of the air sacs, decreasing their ability to recoil. The alveoli then fuse together, decreasing the surface area available for gas exchange.
Patients with emphysema will present with increased functional residual capacity, or FRC, due to the alveolar fusion. They will have hypoxia, V/Q mismatch, and pulmonary hypertension. As the disease advances, the cardiac system will also become involved as the right ventricular afterload is increased, causing right-sided heart failure (cor pulmonale), hypertrophy of the chambers, and decreased left ventricle filling and cardiac output.
Clinically, nurses may expect patients to have dyspnea on exertion and at rest. The patients may experience productive and non-productive coughing, tachypnea, malnutrition, muscle wasting, decreased ventilation (breath sounds), and structural changes to their rib cage (barrel chest). Respiratory testing (PFT) will show a dropping FEV1 and tidal volume. Arterial blood gas testing will show respiratory acidosis that gradually develops metabolic compensation. This means the patient may have a normal pH but have both an increased \(PaO_2\) and \(HCO_3\).
Patients with emphysema are frequently admitted to the acute care facilities due to complications or exacerbations. The most common reasons for acute care admission include pneumonia, heart failure, pulmonary emboli, respiratory failure, bronchospasm, pneumothorax, and decreased or noncompliance in prescribed therapies. Treatment therapies include treating any underlying infection, providing oxygen (as minimally as possible to prevent further perfusion difficulties and dependence), hydration, humidification, secretion breakup and removal, and nutritional support (high calorie, low carbohydrate). Medications that may be used include antibiotics, steroids, bronchodilators, and mucolytics.
COPD
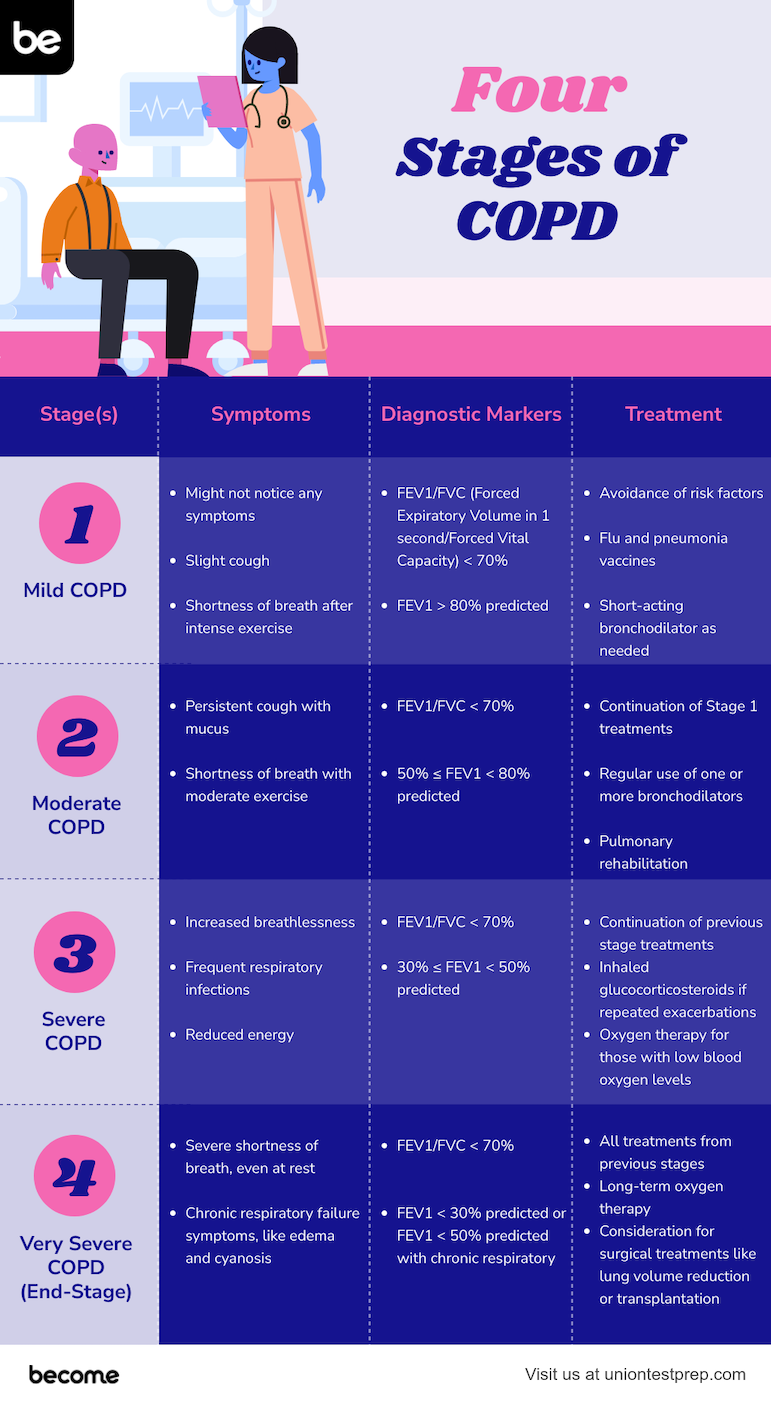
COPD is an irreversible, progressive condition. It can be diagnosed in stages that are determined by a patient’s functional dyspnea, body mass index (BMI), and spirometry. The following are the four stages of COPD:
Stage I— This stage is also known as mild COPD. The patient in this stage will present with or without cough and sputum, but will have some dyspnea. FEV1 will be greater than or equal to 80% of the predicted rate and FEV1:FVC will be less than 70%.
Stage II— This stage is known as moderate COPD. The patient in this stage will present with or without cough and sputum, but will have moderate to severe exertional dyspnea. FEV1 will be between 50-80% of the predicted rate and FEV1:FVC will be less than 70%.
Stage III— This stage is known as severe COPD. The patient in this stage has the same symptoms as stage II; however, the symptoms become repeated and the dyspnea begins to impact the patient’s quality of life. FEV1 will read between 30-50% of the predicted rate and FEV1:FVC will be less than 70%.
Stage IV— This stage is known as severe COPD. It may be life-threatening as severe dyspnea and severe recurrent episodes impact the patient’s quality of life. FEV1 will read at 30% of the predicted rate or less than 50% if the patient has chronic respiratory failure. FEV1:FVC will be less than 70%.
While COPD may not be reversible, it can be managed to reduce pulmonary damage and progressive lung changes. Nurses must provide patient education to help manage this condition. Patients should be instructed on the importance of smoking cessation, being compliant with their prescribed medications, providing pulmonary toileting to reduce secretions, and practicing breathing exercises.
Medications that will likely be considered in COPD include bronchodilators (albuterol and salmeterol), inhaled corticosteroids (Pulmicort®, Vanceril®), and oral corticosteroids (prednisone). In some patients, low-dose oxygen therapy, both during exercise and rest, may be used to provide ventilation support. Surgery may be indicated to remove bullae, reduce lung volume, and, in rare cases, perform a lung transplant.
Chronic Asthma
Asthma is classified by inflammation of the bronchi of the lungs. This is then complicated by the narrowing of pulmonary structures, increased mucus production, and air trapping. The most common symptoms of asthma are cough, wheeze, and dyspnea. In patients with chronic asthma, cough is usually the first, or even only, of these symptoms. Asthma becomes chronic when recurrent bronchospasm and inflammation occur and cause airway remodeling, fibrotic changes, and permanent obstruction.
Chronic asthma may have recurring symptoms of nighttime cough, chest tightness, exertional dyspnea, and daytime cough. While asthma is a chronic condition, acute exacerbations may occur, worsening the airway obstruction. Exacerbations may be triggered by allergies, respiratory viruses, idiosyncratic reactions to NSAID or beta-blocker medication, esophageal reflux, stress, or environmental irritants.
Treatment of asthma includes reducing identified triggers, quick treatment of infections, bronchodilators, long-acting beta-2 agonists, and inhaled glucocorticoids. In some cases, heliox administration may be required to improve oxygen exchange. Sedatives and muscle relaxation may also be used if the patient is unable to achieve control of symptoms.
Status Asthmaticus
Status asthmaticus may occur in those with chronic asthma. It is a severe response of bronchospasm, inflammation, pulmonary obstruction, and decreased ventilation that does not respond to typical asthma therapies. It is usually triggered by a known aggravator such as an allergen, environmental pollution, stress, or exertion. The inflammation worses due to cytokine production from mast cells and T lymphocytes. This increases the blood flow into the lungs, causing fluid accumulation and destruction of the pulmonary lining. This condition is a medical emergency.
Patients in status asthmaticus will present to an acute care facility with these common symptoms: airway obstruction, sternal retractions, intercostal retractions, tachypnea, decreasing oxygen saturations, and forced expiration (tripod positioning). Due to the stress on the lungs, the cardiac system begins to suffer due to increased left ventricular afterload and increased pulmonary edema. If the patient is hypoxic, there may additionally be increased pulmonary vascular resistance and increased right ventricular afterload. Cardiac and respiratory decompensation will occur if not treated quickly.
The patient should be monitored for pulsus paradoxus. Nurses assessing for this condition will notice the patient having a decreased pulse on inspiration and an increased pulse on expiration. If auscultating heart sounds, extra beats with inspiration may be heard. If found, pulsus paradoxus is an indicator for worsening severity of asthma. Arterial blood gas reading on a patient with status asthmaticus will likely show metabolic acidosis. This is classified by a \(PaCO_2\) between 35-45, \(HCO_3\) <22, and pH <7.35.
Treatment for status asthmaticus include the use of beta agonists (albuterol), corticosteroids, and theophylline. Review common medications in these classifications, their indication, and any side effects or contraindications. Rarely, patients with severe status asthmaticus are unable to meet their base perfusion needs and may need to be placed on ECMO (extracorporeal membrane oxygenation) until the lungs have time to recover from the inflammation and damage.
All Study Guides for the CCRN are now available as downloadable PDFs