CCRN Sedation Station
Many patients in the intensive care unit require sedation. Sedation can relieve anxiety and stress while promoting rest and recovery. When utilized properly, it can also reduce negative experiences with hospitalizations or procedures. However, healthcare providers must be careful to avoid overuse of sedation as it may increase risks of delirium, agitation, and substance dependence. Critical care nurses must be familiar with the types of sedation and the reasoning behind their use while caring for patients in the intensive care unit.
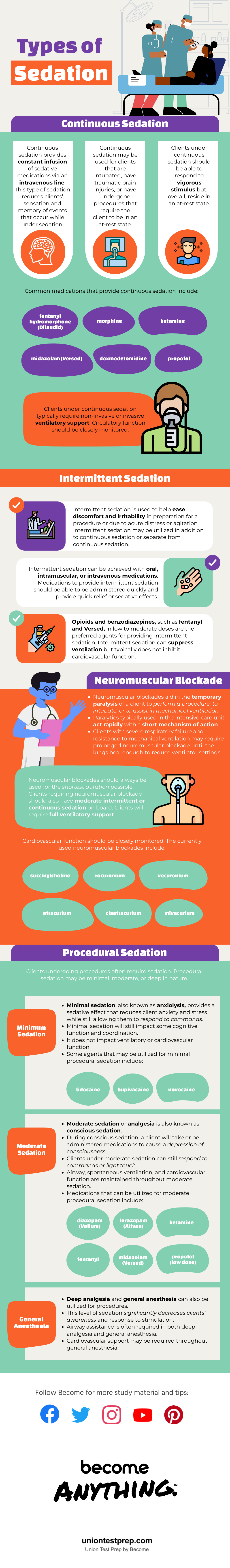
Continuous Sedation
Continuous sedation provides constant infusion of sedative medications via an intravenous line. This type of sedation reduces patients’ sensation and memory of events that occur while under sedation. Continuous sedation may be used for patients that are intubated, have traumatic brain injuries, or have undergone procedures that require the patient to be in an at-rest state. Patients under continuous sedation should be able to respond to vigorous stimulus but, overall, reside in an at-rest state.
Common medications that provide continuous sedation include fentanyl, hydromorphone (Dilaudid), morphine, ketamine, midazolam (Versed), dexmedetomidine, and propofol. Patients under continuous sedation typically require non-invasive or invasive ventilatory support. Circulatory function should be closely monitored.
Intermittent Sedation
Intermittent sedation is used to help ease discomfort and irritability in preparation for a procedure or due to acute distress or agitation. Intermittent sedation may be utilized in addition to continuous sedation or separate from continuous sedation.
Intermittent sedation can be achieved with oral, intramuscular, or intravenous medications. Medications to provide intermittent sedation should be able to be administered quickly and provide quick relief or sedative effects. Opioids and benzodiazepines, such as fentanyl and Versed, in low to moderate doses are the preferred agents for providing intermittent sedation. Intermittent sedation can suppress ventilation but typically does not inhibit cardiovascular function.
Neuromuscular Blockade
Neuromuscular blockades aid in the temporary paralysis of a patient to perform a procedure, to intubate, or to assist in mechanical ventilation. Paralytics typically used in the intensive care unit act rapidly with a short mechanism of action. Patients with severe respiratory failure and resistance to mechanical ventilation may require prolonged neuromuscular blockade until the lungs heal enough to reduce ventilator settings.
Neuromuscular blockades should always be used for the shortest duration possible. Patients requiring neuromuscular blockade should also have moderate intermittent or continuous sedation on board. Patients will require full ventilatory support. Cardiovascular function should be closely monitored. The currently used neuromuscular blockades include succinylcholine, rocuronium, vecuronium, atracurium, cisatracurium, and mivacurium.
Procedural Sedation
Patients undergoing procedures often require sedation. Procedural sedation may be minimal, moderate, or deep in nature.
Minimal Sedation
Minimal sedation, also known as anxiolysis, provides a sedative effect that reduces patient anxiety and stress while still allowing them to respond to commands. Minimal sedation will still impact some cognitive function and coordination. It does not impact ventilatory or cardiovascular function. Some agents that may be utilized for minimal procedural sedation include lidocaine, bupivacaine, and novocaine.
Moderate Sedation
Moderate sedation or analgesia is also known as conscious sedation. During conscious sedation, a patient will take or be administered medications to cause a depression of consciousness. Patients under moderate sedation can still respond to commands or light touch. Airway, spontaneous ventilation, and cardiovascular function are maintained throughout moderate sedation. Medications that can be utilized for moderate procedural sedation include diazepam (Valium), lorazepam (Ativan), ketamine, fentanyl, and midazolam (Versed). Propofol may be utilized in low doses to provide moderate sedation.
General Anesthesia
Deep analgesia and general anesthesia can also be utilized for procedures. This level of sedation significantly decreases patients’ awareness and response to stimulation. Airway assistance is often required in both deep analgesia and general anesthesia. Cardiovascular support may be required throughout general anesthesia.
Nursing Considerations
Critical care nurses provide frontline sedation management. Patients requiring sedation should have their vital signs monitored closely. Nurses should intervene with any concerns for respiratory depression or cardiovascular compromise. Nurses must ensure that the patient has a secure airway, especially when a neuromuscular blockade is introduced.
Patients can be over- or under-sedated. Nurses might have orders to provide sedation boluses as needed. Current guidelines favor reducing the use of sedative medications. This helps prevent delirium and agitation. Overall, nurses must perform regular assessments and advocate for their patients to ensure that their comfort is maximized with the least amount of medication possible.
Keep Reading

CCRN Blog
Is CCRN Certification Worth It?
The CCRN (Critical Care Registered Nurse) Certification stands as a tes…

CCRN Blog
Is the CCRN Exam Hard?
In the US, over 700,000 people work in critical care units (CCUs). With…
CCRN Blog
Traumatic Brain Injury and Intracranial Hemorrhage
Traumatic brain injury and intracranial hemorrhage are two common diagn…