Reduction of Risk Potential Study Guide for the NCLEX-RN Exam
Page 1
Under the umbrella of physiological integrity, risk reduction is critical to improving the safety of patients and current health care practices. Test results, vital signs, and signs of complications will modify courses of treatment to provide the least risk possible to the patient. Below are the main topics covered in this question category.
Vital Signs
A patient’s vital signs are the most rapid assessment tool that one can use to monitor for drastic changes in physiologic function as well as responses to interventions. Changes and abnormalities in heart rate, respiration, blood pressure, temperature, and oxygen saturation can all point to potential and underlying physiological problems.
Assess and Respond
Assessment of vital signs is a valuable tool to determine a patient’s basic physiologic functioning. Because there is often a rapid change in vitals with abnormal physiologic function, the nurse should be able to correlate these changes with knowledge of the patient’s pathophysiology. For example, an increased temperature should alert the nurse to a possible infection.
Basic Values
Temperature
Understand and execute the proper procedure to take a temperature given the patient’s age and conditions. Temperatures may be taken via oral, rectal, tympanic, axillary, or temporal contact depending on the equipment available. Be aware of the impact of emotions, hormonal cycles, and environmental temperatures when obtaining a final value. Normal body temperature is approximately 98.6 degrees Fahrenheit (36.7–37 degrees Centigrade).
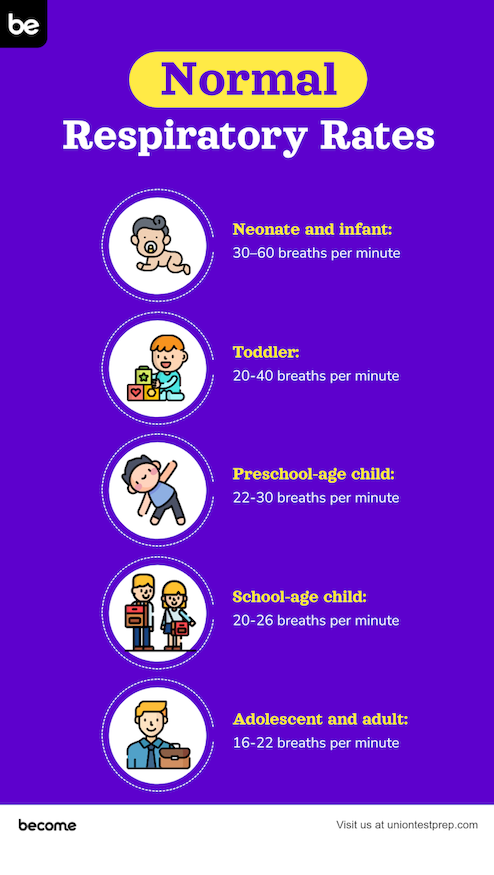
Respirations
Correctly assess the rate, quality, and depth of respirations. Know the normal ranges and sounds for patients of different ages as well as different physiologic changes that can cause a respiratory rate increase or respiratory depression (CNS depression/damage, acidosis/alkalosis, fever, pain, etc.). Normal range of respiratory rate depends on age:
- neonate and infant: 30–60 breaths per minute
- toddler: 20–40 breaths per minute
- preschool-age child: 22–30 breaths per minute
- school-age child: 20–26 breaths per minute
- adolescent and adult: 16–22 breaths per minute
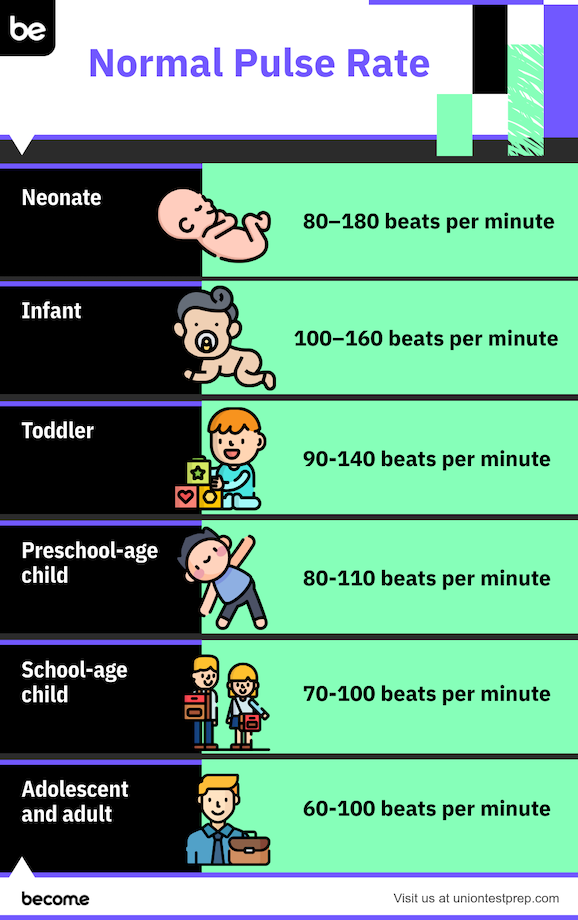
Heart rate
Assess pulses with both palpation and stethoscope auscultation. Know the normal range and how to assess pulse rate based on age specifications. Palpation locations include the radial pulse, femoral pulse, popliteal pulse, dorsalis pedis pulse, posterior tibial pulse, and apical pulse. More central pulse locations (such as the brachial and femoral pulses) should be used to palpate pulses in children. The apical pulse, the pulse point of maximum intensity for an adult, can be located on the left side of the chest at the 5th intercostal space. Assess the quality, regularity, and physiologic symptoms that may influence a pulse rate including cardiovascular changes and autonomic or parasympathetic nervous system activation. Normal pulse ranges include:
- neonate: 80–180 beats per minute
- infant: 100–160 beats per minute
- toddler: 90–140 beats per minute
- preschool-age child: 80-110 beats per minute
- school-age child: 70–100 beats per minute
- adolescent and adult: 60–100 beats per minute
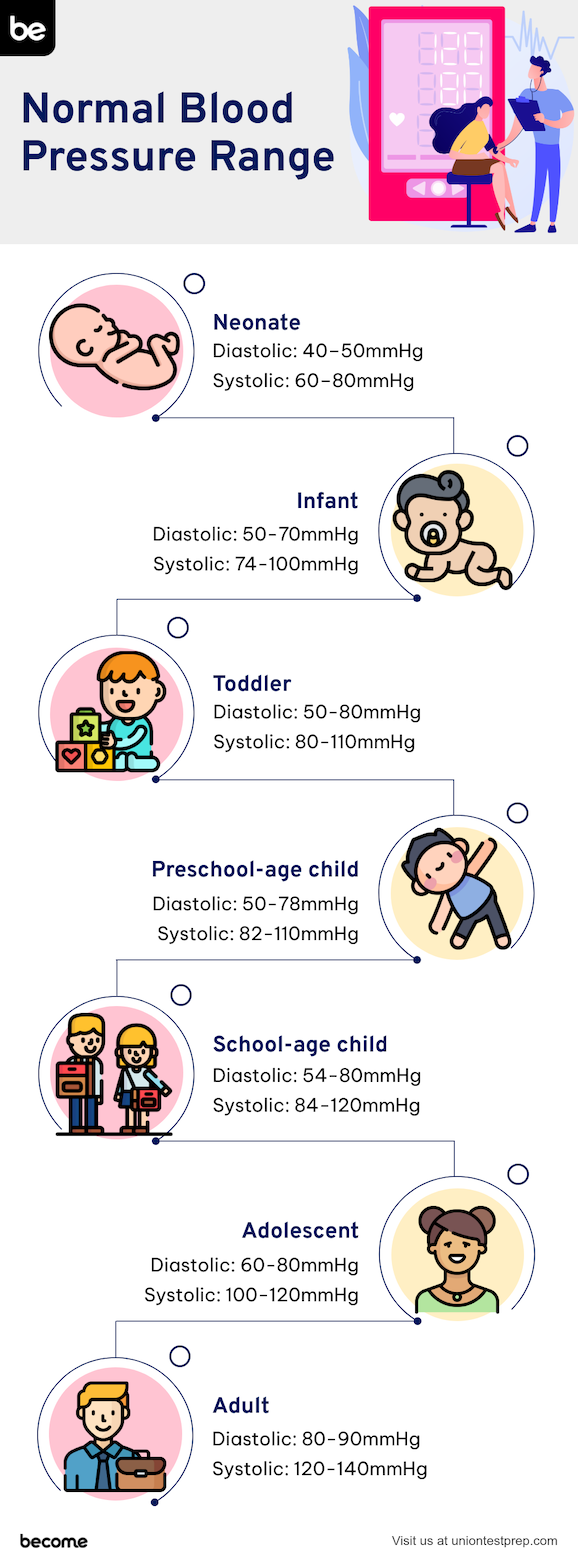
Blood Pressure
Know how to properly measure blood pressure and what underlying physiologic factors affect it (blood volume, cardiac function, the peripheral vascular resistance, blood viscosity, etc.). Know the normal ranges for blood pressure in different age groups along with what phase of the cardiac cycle corresponds with systolic and diastolic pressures. Understand the physiologic systems that can affect or change a patient’s blood pressure (cardiac rate, peripheral vascular resistance, venous return, etc.). Normal blood pressure ranges per age include:
neonate
-
diastolic: 40–50mmHg
-
systolic 60–80mmHg
infant
-
diastolic: 50–70 mmHg
-
systolic 74–100 mmHg
toddler
-
diastolic: 50–80 mmHg
-
systolic 80–110 mmHg
preschool-age child
-
diastolic: 50–78 mmHg
-
systolic 82–110 mmHg
school-age child
-
diastolic: 54–80 mmHg
-
systolic 84–120 mmHg
adolescent
-
diastolic: 60–80 mmHg
-
systolic 100–120 mmHg
adult
- diastolic: 80–90 mmHg
- systolic 120–140 mmHg
Oxygenation
Some patients will need additional monitoring of \(SpO_2\), or percentage of oxygen saturated hemoglobin in the blood. Expected value of oxygenation for all patients is between 95–100%. Oxygenation can be measured by using a pulse oximeter machine. Levels lower than 95% may indicate deterioration of organ and patient status. Monitor this vital sign as indicated.
Invasive Monitoring Data
The vital sign discussion above refers to non-invasive methods of monitoring. Understand the use and rationale for invasive monitoring such as intracranial pressure monitoring and invasive hemodynamic monitoring.
Clinical scenarios in which intracranial pressure monitoring may be required include head trauma, tumor, intracranial bleeding, and stroke. External vital signs for intracranial pressure monitoring include headache, vomiting, pupillary change, and decreased level of consciousness.
Invasive hemodynamic monitoring includes measurements of pulmonary artery pressure, continuous blood pressure monitoring, pulmonary artery wedge pressure, central venous pressure, cardiac output, and intra-arterial pressure. Hemodynamic monitoring is often indicated in any conditions that require close monitoring of hemodynamic status such as septic shock, multiorgan failure, traumatic injury, and cardiac disease exacerbation.
Diagnostic Tests
Diagnostic testing is an essential part of risk reduction, as it may indicate one or more underlying problems that may be addressed with potentially life-saving intervention. Both invasive and non-invasive diagnostic testing is involved in nursing care.
Testing Procedures
Regardless of the diagnostic test being used, the nurse should always employ a general set of testing procedures prior to administering (or assisting with) any diagnostic test. Among these are:
- verification of the test order
- verification of the correct patient using at least two unique identifiers
- providing an explanation and education on the purpose of the test to the patient/family/caregivers along with special instructions (NPO, etc.)
- obtaining/verifying informed consent
- hand washing, universal precautions, aseptic technique, etc. depending on the proper requirements for the test
- proper, complete, and accurate labeling of the specimens along with proper care, storage, and transport
- proper cleanup and disposal of all materials used or collected during the test, including biohazardous waste and proper disposal of other potentially dangerous or caustic materials (preservatives, chemicals, anticoagulants, etc.)
Nursing Knowledge
Always apply knowledge of nursing procedures when administering a diagnostic test. Each test will have a unique set of procedures to follow and psychomotor skills that must be employed. Be familiar with what these are for a wide spectrum of diagnostic testing.
Perform Tests
A nurse must be familiar with the purpose of and preparation for a number of medical tests, including these:
- General tests: biopsies, computed tomography (CT scan), magnetic resonance imaging (MRI), ultrasound, x-ray
- Respiratory tests: pulmonary function tests (PFTs), bronchoscopy, incentive spirometry
- Cardiovascular tests: electrocardiogram (EKG), angiography
- Renal/urinary testing: cystoscopy, intravenous pyelography (IVP), bladder pressure monitoring
- Neurological tests: electroencephalogram (EEG), myelography
- Musculoskeletal tests: bone densitometry, arthroscopy, etc.
- Gastrointestinal tests: colonoscopy, barium enema, glucose monitoring
- Reproductive tests: fetal heart monitoring, non-stress test, amniocentesis, ultrasound, mammogram
- Integumentary tests: tuberculin skin test, allergy testing
Evaluation
Diagnostic test results provide signals for nurses to determine which patients need rapid evaluation. Nurses must compare the newest laboratory or testing results with previous studies to determine any alterations from the patient’s baseline status. Examples of critical diagnostic testing include blood glucose monitoring, oxygen saturation, fecal occult blood, and serum electrolytes. Be familiar with all testing methods in which nursing evaluation is essential to proper care.
In other instances, nurses will be asked to monitor the ongoing results of diagnostic testing. Such tests will likely include maternal-fetal tests such as a non-stress test, amniocentesis, ultrasound, and fetal heart monitoring. Some of these may require you to compare the findings to earlier test data.
Nurses are often the very first member of the healthcare team to become aware of an abnormal result. In some cases, nurses may be able to intervene and/or modify the plan of care to address the issue. On other occasions, they may need to inform the treating practitioner of critical values that may pose an immediate risk of harm to the patient.
Laboratory Values
Understanding the importance of laboratory values, normal laboratory ranges, and proper collection and monitoring techniques is critical to taking proper care of any patient.
Patient Education
Similar to diagnostic testing, nurses will usually prepare the patient for laboratory testing. They will explain the purpose of the test, along with providing education as to what to expect and how the patient should prepare for the test. Nursing education may also involve instructing patients on which laboratory testing will be required with the patient’s chronic illnesses and/or prescribed medications. Examples of this include diabetic patients having daily glucose monitoring and routine A1C testing and patients taking Coumadin (Warfarin) requiring regularly scheduled coagulation studies.
Obtaining Specimens
Be familiar with the proper technique and the steps to collect blood specimens from both a peripheral vein and a central venous catheter. Know how to properly collect specimens from a wound (generally a swab specimen), as well as stool (routine, guaiac, and infectious) and urine (routine, clean catch, midstream and timed).
Specimen Values
While it may be impossible to memorize the normal ranges for every laboratory specimen, it is very helpful to have knowledge of what the general, normal range is for the most commonly ordered laboratory tests. The following lab tests are some of the most commonly ordered tests:
- Arterial blood gas or ABG: (\(pH\), \(PO_2\), \(PCO_2\), \(SaO_2\), \(HCO_3\))
- Lipid levels: (total cholesterol, triglycerides, high density lipoprotein or HDL, low density lipoprotein or LDL)
- Glucose: (fasting, random, glycosylated hemoglobin or \(HgbA_1C\))
- Complete blood count or CBC: (white blood cells or WBCs, hematocrit, hemoglobin, platelets)
- Basic metabolic or electrolyte panel: (sodium, potassium, magnesium, chloride, calcium, carbon dioxide, glucose, etc.)
- Renal indices: (creatinine, blood urea nitrogen or BUN)
- Coagulation studies: (prothrombin time or PT, partial thromboplastin time or PTT, activated partial thromboplastin time or aPTT, international normalized ratio or INR)
In addition to knowing the normal ranges for these tests, the nurse will need to critically evaluate the patient’s laboratory values. Monitor every lab result, evaluate for changes, and correlate the findings with the patient’s condition and any previous lab results and/or interventions.
Notification
The nurse is often the first to receive and review laboratory results. The nurse must then notify the ordering and primary care practitioners of any abnormal results.
All Study Guides for the NCLEX-RN Exam are now available as downloadable PDFs