Cardiovascular Study Guide for the CCRN
Page 1
General Information
On the CCRN® test, you will see that about 18% of the questions concern making decisions about cardiovascular issues while in a critical care nursing position. The questions all begin with a scenario and you’ll need to rely on a vast amount of knowledge about not only the anatomy of the cardiovascular system but also what to do if things aren’t functioning properly and methods of addressing emergency situations in this realm. This study guide will review the basics that will be assessed on the test.
Acute Coronary Syndromes
Acute coronary syndromes occur in the event that blood flow is lost, intermittently or permanently, causing cardiac muscle damage, ischemia, and injury. There are several types of acute coronary syndrome. Please review these diagnoses, risk factors, prevention strategies, and therapies:
Non-ST Segment Elevation Myocardial Infarction (NSTEMI)
Two common classifications of myocardial infarction exist. The first to review is the non-ST segment elevation myocardial infarction (NSTEMI). In the event of a NSTEMI, circulation is reduced and not completely blocked. Changes on ECG show a depressed ST wave or T wave inversion with no progression to Q wave. There will be a partial blockage of the coronary artery noted on cardiac catheterization. In some events, a cardiac stent will be placed to support the vessel and in others, balloon angioplasty may be performed to compress the plaques and reduce the blocked area.
See the section on Myocardial Infarction/Ischemia for more information regarding the diagnosis and treatment of this condition.
ST Segment Elevation Myocardial Infarction (STEMI)
The second myocardial infarction type to review is the ST segment elevation myocardial infarction (STEMI). STEMI events occur when a blockage occurs, limiting or stopping blood circulation to the cardiac muscle. The ECG will show an elevated ST wave with progression to the Q wave. There will be full blockage of the coronary artery and, depending on the density of the blockage, either a cardiac stent or cardiac bypass surgery will be performed to restore circulation to the distal tissues.
See the section on Myocardial Infarction/Ischemia for more information regarding the diagnosis and treatment of this condition.
Stable Angina
Stable angina is chest pain that occurs with stress or exercise and is a result of decreased blood flow through the heart. Symptoms include dyspnea, diaphoresis, dizziness, fatigue, nausea, and anxiety. It can be diagnosed by angiogram and by performing a stress test. Risk factors for stable angina include diabetes, high blood pressure, hyperlipidemia, sedentary lifestyle, smoking, older age, and male gender. This type of angina is relieved by rest and/or nitroglycerin. Medications and/or lifestyle changes to manage the underlying chronic conditions/risk factors should also be considered.
Unstable Angina
Also called preinfarction or crescendo angina, unstable angina is chest pain that occurs both at rest and with exertion. The pain gradually worsens and becomes more frequent, eventually leading to a myocardial infarction (heart attack). Symptoms of unstable angina are the same as stable angina. Risk factors include diabetes, obesity, family history, hypertension, hyperlipidemia, male gender, smoking history, and an inactive lifestyle. Age is also a risk factor. Men over the age of 45 and women over the age of 55 are more at risk for unstable angina. Diagnosis can be completed with lab work (creatine kinase, troponin, etc.), electrocardiogram (ECG), echocardiography (echo), and CT angiography (CTA). Treatment includes eliminating or reducing the blockage, antiplatelet therapy (heparin, Lovenox®, warfarin, clopidogrel, etc.), and medications to treat any underlying chronic conditions. Lifestyle changes, including a low-sodium diet, lowering stress, increasing exercise, losing weight (if overweight), and stopping smoking, are also recommended.
Variant Angina
Also known as Prinzmetal’s angina, variant angina occurs at rest and rarely with exertion and is a result of epicardial coronary artery spasm. It usually happens in the night or early morning hours. Diagnosis is confirmed with ergonovine or acetylcholine administration during angiography. This helps to visualize the active spasm. ST segment elevation on ECG may occur during the spasms. Treatment of this condition is with calcium channel blockers and nitroglycerin. Beta-blockers may exacerbate spasm and should be avoided. Prognosis with treatment is good.
Acute Myocardial Infarction/Ischemia
Acute myocardial infarction/ischemia (MI) is commonly known as a heart attack. MIs occur due to the blockage of blood flow through some of the heart, resulting in death of the cardiac muscles.
Causes and Symptoms
This may be due to either embolus or vasospasm. While previous cardiovascular disease may have been identified, many patients have no prior cardiac history. Common symptoms of acute MI include pain to the neck or arms, palpitations, hypertension or hypotension, pulmonary edema, nausea, vomiting, diaphoresis, neurologic disturbances, visual changes, speech changes, and feelings of dread or doom.
Diagnosis
Early diagnosis is key to implementing life-saving measures. Electrocardiogram (ECG) tracings may identify T wave inversion, elevated ST segments, abnormal Q waves, tachycardia, bradycardia, or dysrhythmias. An echocardiogram may be used to assess ventricular function and identify any concerns in blood flow/perfusion. Numerous blood tests should also be performed. The following are the most commonly drawn labs after a MI:
-
Troponin levels— increase three to six hours after infarct, peak at 14 to 20 hours, and are elevated for one to 2 weeks
-
Creatine kinase (CK-MB)— increases four to eight hours after injury and peaks at 24 hours (earlier with thrombolytic therapy)
-
Ischemia modified albumin (IMA)— increases in minutes, peaks at six hours, and returns to baseline
-
Myoglobin— increases in 30 minutes to four hours, peaks at six to seven hours, and a failure to increase can be used to rule out MI
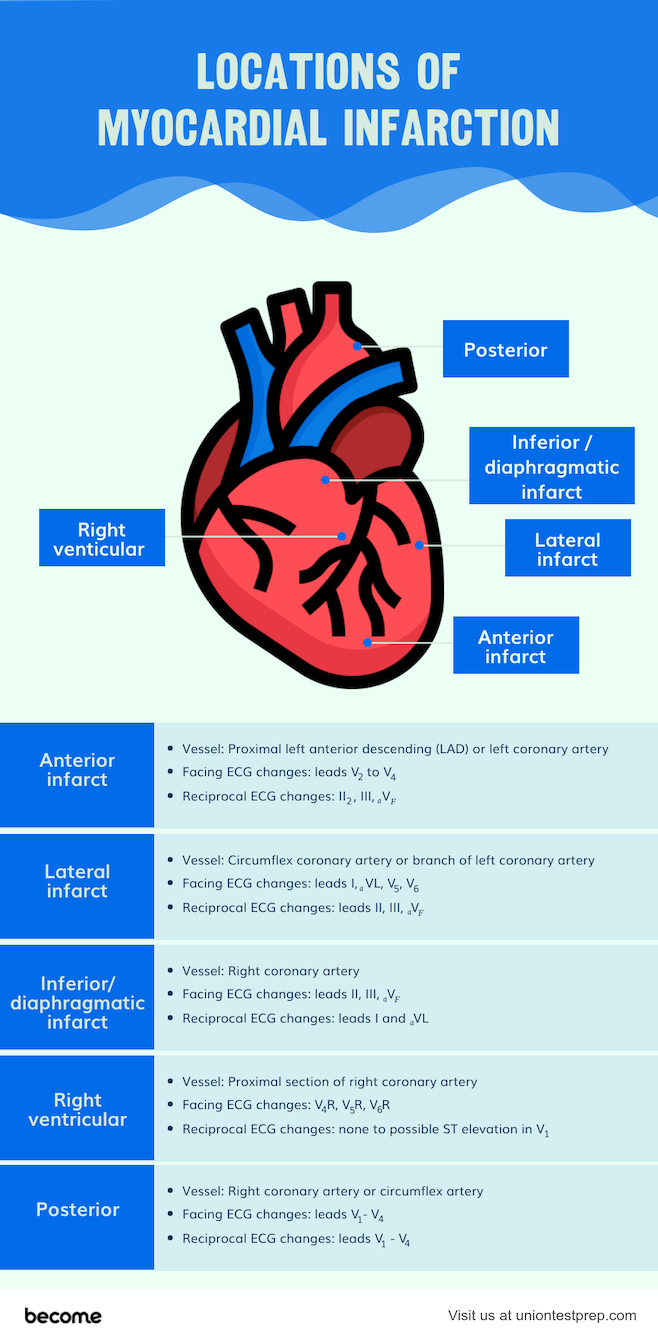
Locations of MI
The most common locations for MI, either STEMI or NSTEMI, are in the left ventricle and septum. However, occlusions can occur in other coronary vessels that may result in right ventricular ischemia. Nurses should understand the association between vessel occlusion and resulting infarct location. Also note which leads to monitor for ECG changes in that patient.
- Anterior infarct
- Vessel: Proximal left anterior descending (LAD) or left coronary artery
- Facing ECG changes: leads \(V_2\) to \(V_4\)
- Reciprocal ECG changes: II, III, \(_aV_F\)
- Lateral infarct
- Vessel: Circumflex coronary artery or branch of left coronary artery
- Facing ECG changes: leads I, \(_aVL\), \(V_5\), \(V_6\)
- Reciprocal ECG changes: leads II, III, \(_aV_F\)
- Inferior/diaphragmatic infarct
- Vessel: Right coronary artery
- Facing ECG changes: leads II, III, \(_aV_F\)
- Reciprocal ECG changes: leads I and \(_aVL\)
- Right ventricular
- Vessel: Proximal section of right coronary artery
- Facing ECG changes: \(V_4R\), \(V_5R\), \(V_6R\)
- Reciprocal ECG changes: none to possible ST elevation in \(V_1\)
- Posterior
- Vessel: Right coronary artery or circumflex artery
- Facing ECG changes: leads \(V_1 - V_4\)
- Reciprocal ECG changes: leads \(V_1−V_4\)
Treatment for MI
Treatment for acute MI may take several forms. Depending on the degree and location of the blockage, MI symptoms may be treated with cardiac catheterization, vessel stenting, and medication. Open heart surgery, bypass procedure, and extended infusions are also treatment options if previous methods do not adequately restore circulation.
Fibrinolytic infusions may be indicated if symptoms of MI have been occurring for less than 12 hours, have greater than or equal to 1 mm elevation of ST tracing in greater than two contiguous leads, and have no contraindications or cardiogenic shock. The earlier the administration of these agents, the better the outcome. Common medications include first-generation fibrinolytics streptokinase and anistreplase, second-generation alteplase or tissue plasminogen activator (tPA), and third-generation reteplase and tenecteplase.
Contraindications to fibrinolytic therapy include history of severe bleeding, intracranial hemorrhage, history of stroke, aortic dissection, pericarditis, recent (<3 months) spinal or cranial surgery, neoplasm, aneurysm, or AVM. High caution should be used in patients with active peptic ulcer, renal or hepatic disease, pregnancy, anticoagulation therapy, uncontrolled hypertension, recent (in past two to four weeks) internal bleeding, and greater than 10 minutes of CPR.
Continual monitoring of labs and need for continued fibrinolytic therapy should be performed. In the event of cardiac surgery or catheterization, follow postoperative recommendations to prevent bleeding, and monitor for hemorrhage and other potential complications.
All Study Guides for the CCRN are now available as downloadable PDFs