Ventilation Comprehension
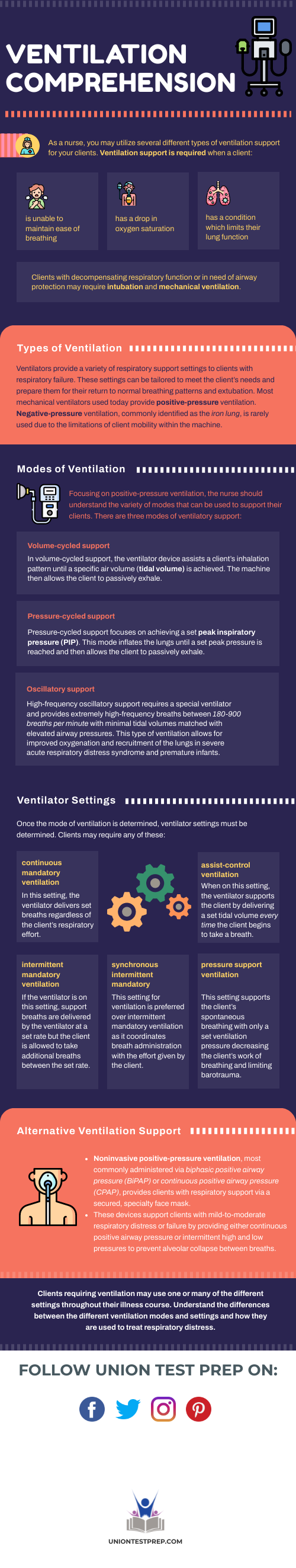
As a nurse, you may utilize several different types of ventilation support for your patients. Ventilation support is required when a patient:
- is unable to maintain ease of breathing
- has a drop in oxygen saturation
- has a condition which limits their lung function
Patients with decompensating respiratory function or in need of airway protection may require intubation and mechanical ventilation.
Types of Ventilation
Ventilators provide a variety of respiratory support settings to patients with respiratory failure. These settings can be tailored to meet the patient’s needs and prepare them for their return to normal breathing patterns and extubation. Most mechanical ventilators used today provide positive-pressure ventilation. Negative-pressure ventilation, commonly identified as the iron lung, is rarely used due to the limitations of patient mobility within the machine.
Modes of Ventilation
Focusing on positive-pressure ventilation, the nurse should understand the variety of modes that can be used to support their patients. There are three modes of ventilatory support:
Volume-cycled support
In volume-cycled support, the ventilator device assists a patients inhalation pattern until a specific air volume (tidal volume) is achieved. The machine then allows the patient to passively exhale.
Pressure-cycled support
Pressure-cycled support focuses on achieving a set peak inspiratory pressure (PIP). This mode inflates the lungs until a set peak pressure is reached and then allows the patient to passively exhale.
Oscillatory support
High-frequency oscillatory support requires a special ventilator and provides extremely high-frequency breaths between 180-900 breaths per minute with minimal tidal volumes matched with elevated airway pressures. This type of ventilation allows for improved oxygenation and recruitment of the lungs in severe acute respiratory distress syndrome and premature infants.
Ventilator Settings
Once the mode of ventilation is determined, ventilator settings must be determined. Patients may require any of these:
Continuous mandatory ventilation
In this setting, the ventilator delivers set breaths regardless of the patient’s respiratory effort.
Assist-control ventilation
When on this setting, the ventilator supports the patient by delivering a set tidal volume every time the patient begins to take a breath.
Intermittent mandatory ventilation
If the ventilator is on this setting, support breaths are delivered by the ventilator at a set rate but the patient is allowed to take additional breaths between the set rate.
Synchronous intermittent mandatory
This setting for ventilation is preferred over intermittent mandatory ventilation as it coordinates breath administration with the effort given by the patient.
Pressure support ventilation
This setting supports the patient’s spontaneous breathing with only a set ventilation pressure decreasing the patient’s work of breathing and limiting barotrauma.
Alternative Ventilation Support
Noninvasive positive-pressure ventilation, most commonly administered via biphasic positive airway pressure (BiPAP) or continuous positive airway pressure (CPAP), provides patients with respiratory support via a secured, specialty face mask. These devices support patients with mild-to-moderate respiratory distress or failure by providing either continuous positive airway pressure or intermittent high and low pressures to prevent alveolar collapse between breaths.
Patients requiring ventilation may use one or many of the different settings throughout their illness course. Understand the differences between the different ventilation modes and settings and how they are used to treat respiratory distress. For more in-depth study material on ventilation or other CCRN concepts, check out our CCRN practice tests, study guides, and flashcards.
Keep Reading

CCRN Blog
Is CCRN Certification Worth It?
The CCRN (Critical Care Registered Nurse) Certification stands as a tes…

CCRN Blog
Is the CCRN Exam Hard?
In the US, over 700,000 people work in critical care units (CCUs). With…
CCRN Blog
Traumatic Brain Injury and Intracranial Hemorrhage
Traumatic brain injury and intracranial hemorrhage are two common diagn…