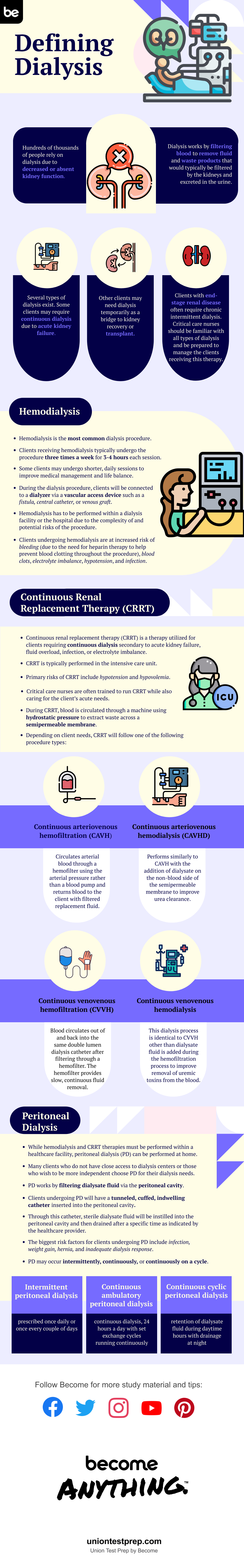
Defining Dialysis
Hundreds of thousands of people rely on dialysis due to decreased or absent kidney function. Dialysis works by filtering blood to remove fluid and waste products that would typically be filtered by the kidneys and excreted in the urine.
Several types of dialysis exist. Some patients may require continuous dialysis due to acute kidney failure. Other patients may need dialysis temporarily as a bridge to kidney recovery or transplant. Patients with end-stage renal disease often require chronic intermittent dialysis. Critical care nurses should be familiar with all types of dialysis and be prepared to manage the patients receiving this therapy.
Hemodialysis
Hemodialysis is the most common dialysis procedure. Patients receiving hemodialysis typically undergo the procedure three times a week for 3-4 hours each session. Some patients may undergo shorter, daily sessions to improve medical management and life balance.
During the dialysis procedure, patients will be connected to a dialyzer via a vascular access device such as a fistula, central catheter, or venous graft. Hemodialysis has to be performed within a dialysis facility or the hospital due to the complexity of and potential risks of the procedure. Patients undergoing hemodialysis are at increased risk of bleeding (due to the need for heparin therapy to help prevent blood clotting throughout the procedure), blood clots, electrolyte imbalance, hypotension, and infection.
Continuous Renal Replacement Therapy (CRRT)
Continuous renal replacement therapy (CRRT) is a therapy utilized for patients requiring continuous dialysis secondary to acute kidney failure, fluid overload, infection, or electrolyte imbalance. CRRT is typically performed in the intensive care unit. Primary risks of CRRT include hypotension and hypovolemia. Critical care nurses are often trained to run CRRT while also caring for the patient’s acute needs.
During CRRT, blood is circulated through a machine using hydrostatic pressure to extract waste across a semipermeable membrane. Depending on patient needs, CRRT will follow one of the following procedure types:
-
Continuous arteriovenous hemofiltration (CAVH)—circulates arterial blood through a hemofilter using the arterial pressure rather than a blood pump and returns blood to the patient with filtered replacement fluid.
-
Continuous arteriovenous hemodialysis (CAVHD)—performs similarly to CAVH with the addition of dialysate on the non-blood side of the semipermeable membrane to improve urea clearance.
-
Continuous venovenous hemofiltration (CVVH)—blood circulates out of and back into the same double lumen dialysis catheter after filtering through a hemofilter. The hemofilter provides slow, continuous fluid removal.
-
Continuous venovenous hemodialysis—this dialysis process is identical to CVVH other than dialysate fluid is added during the hemofiltration process to improve removal of uremic toxins from the blood.
Peritoneal Dialysis
While hemodialysis and CRRT therapies must be performed within a healthcare facility, peritoneal dialysis (PD) can be performed at home. Many patients who do not have close access to dialysis centers or those who wish to be more independent choose PD for their dialysis needs.
PD works by filtering dialysate fluid via the peritoneal cavity. Patients undergoing PD will have a tunneled, cuffed, indwelling catheter inserted into the peritoneal cavity. Through this catheter, sterile dialysate fluid will be instilled into the peritoneal cavity and then drained after a specific time as indicated by the healthcare provider. The biggest risk factors for patients undergoing PD include infection, weight gain, hernia, and inadequate dialysis response.
PD may occur intermittently, continuously, or continuously on a cycle.
-
Intermittent peritoneal dialysis—prescribed once daily or once every couple of days
-
Continuous ambulatory peritoneal dialysis—continuous dialysis, 24 hours a day with set exchange cycles running continuously
-
Continuous cyclic peritoneal dialysis—retention of dialysate fluid during daytime hours with drainage at night
Many patients in critical care units will already utilize or need dialysis for the management of kidney injury and end-stage renal disease. Critical care nurses should have a general understanding of each type of dialysis and their purposes to best care for their patients requiring this medical treatment. For more in-depth information on dialysis and other critical care nursing concepts, or to test your knowledge, check out our practice tests, study guides, and flashcards for the CCRN.
Keep Reading

CCRN Blog
Is CCRN Certification Worth It?
The CCRN (Critical Care Registered Nurse) Certification stands as a tes…

CCRN Blog
Is the CCRN Exam Hard?
In the US, over 700,000 people work in critical care units (CCUs). With…
CCRN Blog
Traumatic Brain Injury and Intracranial Hemorrhage
Traumatic brain injury and intracranial hemorrhage are two common diagn…