Classifying Strokes and Critical Stroke Care
Stroke is one of the leading causes of death in the United States. Many patients who experience a stroke will be cared for in the intensive care unit. Early identification of the stroke allows for critical intervention and treatment measures. Early stroke management helps to reduce patient mortality.
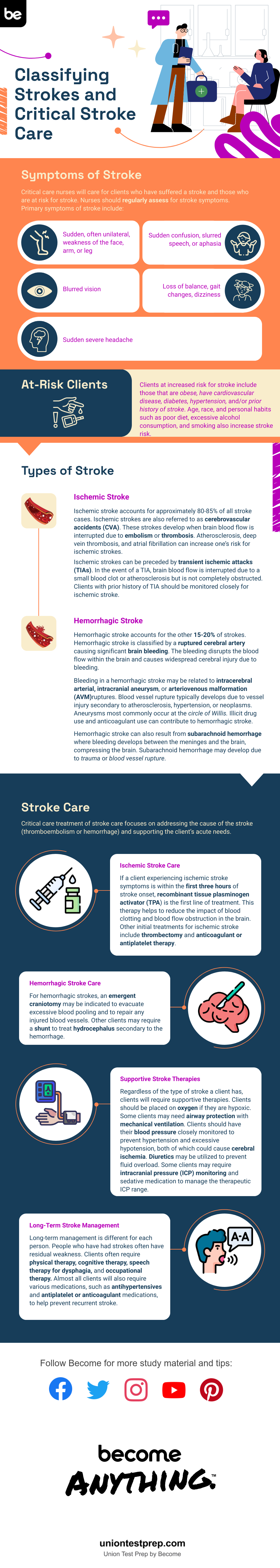
Symptoms of Stroke
Critical care nurses will care for patients who have suffered a stroke and those who are at risk for stroke. Nurses should regularly assess for stroke symptoms. Primary symptoms of stroke include:
- Sudden, often unilateral, weakness of the face, arm, or leg
- Sudden confusion, slurred speech, or aphasia
- Blurred vision
- Loss of balance, gait changes, dizziness
- Sudden severe headache
At-Risk Patients
Patients at increased risk for stroke include those that are obese, have cardiovascular disease, diabetes, hypertension, and/or prior history of stroke. Age, race, and personal habits such as poor diet, excessive alcohol consumption, and smoking also increase stroke risk.
Types of Stroke
Ischemic Stroke
Ischemic stroke accounts for approximately 80-85% of all stroke cases. Ischemic strokes are also referred to as cerebrovascular accidents (CVA). These strokes develop when brain blood flow is interrupted due to embolism or thrombosis. Atherosclerosis, deep vein thrombosis, and atrial fibrillation can increase one’s risk for ischemic strokes.
Ischemic strokes can be preceded by transient ischemic attacks (TIAs). In the event of a TIA, brain blood flow is interrupted due to a small blood clot or atherosclerosis but is not completely obstructed. Patients with prior history of TIA should be monitored closely for ischemic stroke.
Hemorrhagic Stroke
Hemorrhagic stroke accounts for the other 15-20% of strokes. Hemorrhagic stroke is classified by a ruptured cerebral artery causing significant brain bleeding. The bleeding disrupts the blood flow within the brain and causes widespread cerebral injury due to bleeding.
Bleeding in a hemorrhagic stroke may be related to intracerebral arterial, intracranial aneurysm, or arteriovenous malformation (AVM) ruptures. Blood vessel rupture typically develops due to vessel injury secondary to atherosclerosis, hypertension, or neoplasms. Aneurysms most commonly occur at the circle of Willis. Illicit drug use and anticoagulant use can contribute to hemorrhagic stroke.
Hemorrhagic stroke can also result from subarachnoid hemorrhage where bleeding develops between the meninges and the brain, compressing the brain. Subarachnoid hemorrhage may develop due to trauma or blood vessel rupture.
Stroke Care
Critical care treatment of stroke care focuses on addressing the cause of the stroke (thromboembolism or hemorrhage) and supporting the patient’s acute needs.
Ischemic Stroke Care
If a patient experiencing ischemic stroke symptoms is within the first three hours of stroke onset, recombinant tissue plasminogen activator (TPA) is the first line of treatment. This therapy helps to reduce the impact of blood clotting and blood flow obstruction in the brain. Other initial treatments for ischemic stroke include thrombectomy and anticoagulant or antiplatelet therapy.
Hemorrhagic Stroke Care
For hemorrhagic strokes, an emergent craniotomy may be indicated to evacuate excessive blood pooling and to repair any injured blood vessels. Other patients may require a shunt to treat hydrocephalus secondary to the hemorrhage.
Supportive Stroke Therapies
Regardless of the type of stroke a patient has, patients will require supportive therapies. Patients should be placed on oxygen if they are hypoxic. Some patients may need airway protection with mechanical ventilation. Patients should have their blood pressure closely monitored to prevent hypertension and excessive hypotension, both of which could cause cerebral ischemia. Diuretics may be utilized to prevent fluid overload. Some patients may require intracranial pressure (ICP) monitoring and sedative medication to manage the therapeutic ICP range.
Long-Term Stroke Management
Long-term management is different for each person. People who have had strokes often have residual weakness. Patients often require physical therapy, cognitive therapy, speech therapy for dysphagia, and occupational therapy. Almost all patients will also require various medications, such as antihypertensives and antiplatelet or anticoagulant medications, to help prevent recurrent stroke.
Critical care nurses will frequently experience caring for patients with strokes. Be prepared to identify symptoms, assess patients, assist in treatment, and help through the recovery of these patients. For more information on strokes and other critical care concepts, or to test your knowledge, check out our free CCRN practice tests, study guides, and flashcards.
Keep Reading

CCRN Blog
Is CCRN Certification Worth It?
The CCRN (Critical Care Registered Nurse) Certification stands as a tes…

CCRN Blog
Is the CCRN Exam Hard?
In the US, over 700,000 people work in critical care units (CCUs). With…
CCRN Blog
Traumatic Brain Injury and Intracranial Hemorrhage
Traumatic brain injury and intracranial hemorrhage are two common diagn…